To mark International Women’s Day and Women’s History Month,
we delivered a presentation for NHS Lothian’s Women’s Network to highlight the instrumental
role of two pioneering women who held very different roles but whose career
paths converged in the mid-1980s to tackle a major health crisis. The theme for
this year's IWD is #AccelerateAction and, with this in view, Dr
Helen Zealley and Dr Jacqueline Mok played an essential part in establishing a response to critical
issues that affected the health and wellbeing of the people in Lothian.
Dr Helen Zealley completed her studies in Medicine at the
University of Edinburgh. In the 1970s, she became involved with the emerging speciality
of Community Medicine, specialising in Maternal and Child Health within the
children’s service of the Edinburgh Public Health Department for 10 years. She
was appointed Director of Public Health (DPH) – also known as the Chief
Administrative Medical Officer (CAMO) – of Lothian Health Board, which later
became NHS Lothian in 1998, and Executive Director of LHB in 1991, a post she
held until her retirement. During her career, she encountered challenging
periods for Lothian Health Board, such as initiatives to combat the high rate
of HIV infection in Edinburgh and a financial crisis in the early 1990s.
As the Director of Public Health, Dr Zealley was involved,
directly or indirectly, in all the developmental aspects of Lothian Health
Board during the period. These included policies, strategic planning processes
and frameworks, service provision, operational plans, efficiency savings, and auditing…
all of which are evidenced in our archive.
LHB Smoking Policy, Promotional leaflet (GD25/1/1/1/2)
LHB Smoking Policy, 'Smoking Prevention, A Health Promotion Guide for the NHS' promotional booklet (GD25/1/1/1/2)
However, the hardest challenge she
had to face, at least during the first years of her tenure, was the
government’s white paper Working for patients published in January 1989.
In short, 1990 was a year of significant change and turbulence for the NHS both
nationally and locally since a new form of healthcare was established whereby
health services and long-term care were to be planned and managed as a
competitive market. Within this system, Health Boards were to assess the
“health needs” of the population for which they are responsible and place
contracts to “purchase” services to meet those needs from a range of
“providers”, both locally and on a national basis, who were responsible for the
day-to-day management of these services. NHS hospitals and clinics were also
given the opportunity to opt out of their direct management links with Health
Boards and form “self-governing trusts”.
Pamphlets like this were created as a response to the government's 1989 White Paper (GD25/1/1/1/23)
Dr Zealley was not onboard with this new form of healthcare
as the right means to achieve improved service delivery and provision within
the NHS. As she stated in a letter written to an external healthcare agency,
‘my problem is that I do not believe that the purchaser/provider split is a
useful mechanism to achieve this – and I am deeply distressed by the signs of
“competition” between our provider units amongst whom we have spent years
developing a collaborative, integrated approach so that patients receive the
most appropriate “package” of preventive, acute and rehabilitative care –
irrespective of the provider of each component’. While she expresses a clear
openness to change, she opposes the privatisation of health services. Dr
Zealley was a leader, an influential woman, and a real decision-maker. Yet,
although she held a prominent position within the structure of LHB, decisions
dictated by the higher ups, or the Tory government in this case, escaped her
control.

Excerpt from Dr Helen Zealley's letter to an external healthcare body in response to the government's White Paper (GD25/1/1/1/23)
Cartoon published in a newspaper critiquing the government's White Paper (GD25/1/1/1/23)
The reform resonated across the UK and received
substantial media coverage, leading, unsurprisingly, to major disagreement and
backlash from the Labour party. Their main claim was that the government’s
‘ideologically-driven view of healthcare as another commodity to be bought and
sold in a marketplace, rather than a public service’ sought to benefit only a
small portion of the population. While aspects such as poverty, unemployment,
poor housing, and a polluted environment are essential to determine people’s
health, the two-tier system established in the early 1990s resulted in that two
patients with the same disease living in the same street and the same
circumstances could be treated differently depending on what particular type of
doctor they happened to have. This may well give an idea of the convoluted
scenario in which Helen Zealley worked during the 1990s and how her role was
impacted by the country’s political fabric.

Cover page of The Edinburgh and Lothians Post (published on week ending Saturday, 19 October 1991) (GD25/1/1/1/23)
Page from BMA News Review (January 1990) (GD25/1/1/1/23)
A few years before this, Dr Helen Zealley joined forces with
Dr Jacqueline Mok to address the HIV/AIDS crisis affecting Edinburgh from the
mid-1980s. Originally from Malaysia, from where she came from to complete her
Medicine studies in Edinburgh, she was a Paediatric Consultant for Community
Health, Lothian Health Board, as well as a member of the Royal College of
Paediatrics and Children’s Health. Her research mostly focused on HIV and AIDS
in infants and children, with a particular focus on mother-to-child
transmissions. She worked extensively on research for HIV therapies that are
not only safe for children, but also for expectant mothers. Her research
expanded beyond HIV-infected children to include HIV-affected children.
That is, children whose mothers were HIV positive. Dr Mok started a clinic for
HIV-infected children at the City Hospital in the mid-1980s, the first of its
kind in the UK. The clinic moved from this space and was granted use of Ward 8
(Ward for Infectious Diseases) at the Royal Hospital for Sick Children.
In October 1985, she was asked by Dr Helen Zealley to look
after children born to women with HIV infection. At this time, Edinburgh was
the first city in the UK to recognise that HIV could affect the non-gay
community and that it was drug use that resulted in heterosexual spread; a
third of drug users being young women of reproductive age. The uniqueness of
Edinburgh in comparison to other places was that many young heterosexual men
and women were HIV positive, but not ill.
Reducing Mother to Child Transmission of HIV Infection in the United Kingdom, April 1998 (GD59/1/2/3/2)
Dr Mok travelled to New York, New Jersey, and Miami to learn
about the services that had been set up in these places, which were described
as paediatric AIDS by Dr Arye Rubinstein in 1983. He established that
transmission of AIDS can occur in utero and published his findings in 1986.
After her trip, Dr Mok acknowledged that the HIV/AIDS programme in Edinburgh
could benefit from her respiratory background since many children would present
with pneumocystis.
The first reports of paediatric AIDS in 1983 talked about an
acute life-threatening illness with a high level of mortality. When they
eventually got that link of mother-to-child transmission, it was thought to be
as high as 50% to 80%. It was almost certain that if you had a mother with HIV,
you were likely to be infected, and then if you were infected, you would be
dead within the first 5 years of life. However, paediatric AIDS turned out to
be a long-term condition and not every child was going to be infected. The
transmission rate they found from mother-to-child was less than 10%. And from
those children with HIV in Edinburgh, many of them were very well, even before
the days of antiretroviral therapy.
On the other hand, Jacqui encountered some adversity within
NHS staff. When she was asked to set up a clinic for these children, a
colleague told her, “Well, I hope you don’t share their cups with them,
Jacqui!”, whereas somebody else asked her to keep the clinic at City Hospital
as opposed to Sick Kids, where she was based at the time. This gives an idea of
the high level of anxiety experienced by everyone. It was all doom and gloom.
Nothing was known about transmission, which could be relatable to those who
didn’t live through this crisis, but experienced the Covid-19 pandemic.
Community Child Health Research Report (GD59/1/1/5)
At the time of establishing
this clinic at City Hospital, there was only one Ward for Children and all
paediatric trainees were at Sick Kids with no rotation into City Hospital. Dr
Mok would be called because they had no junior doctors who could assess the
children. To exemplify, if they needed an intravenous infusion, she had to go
and do it herself because the trainees were adult-trained. As for her team, it
consisted of Dr Mok (half time), an MRC- funded research fellow for 3 years who
was then replaced by a trainee, a paediatric trainee, a full-time health
visitor, and a secretary working 17.5h. They were eventually joined by an
obstetrician and a specialised midwife as well.
In 1989, she attended her first HIV international conference
and as a result of meeting other paediatricians and epidemiologists, they
started the European Collaborative Study (ECS), for mother-to-child
transmission of HIV. In its hayday, Dr Mok received referrals from Edinburgh
and the Lothian, Fife, Tayside, the Borders, the Highlands and Islands, and
even northern England.
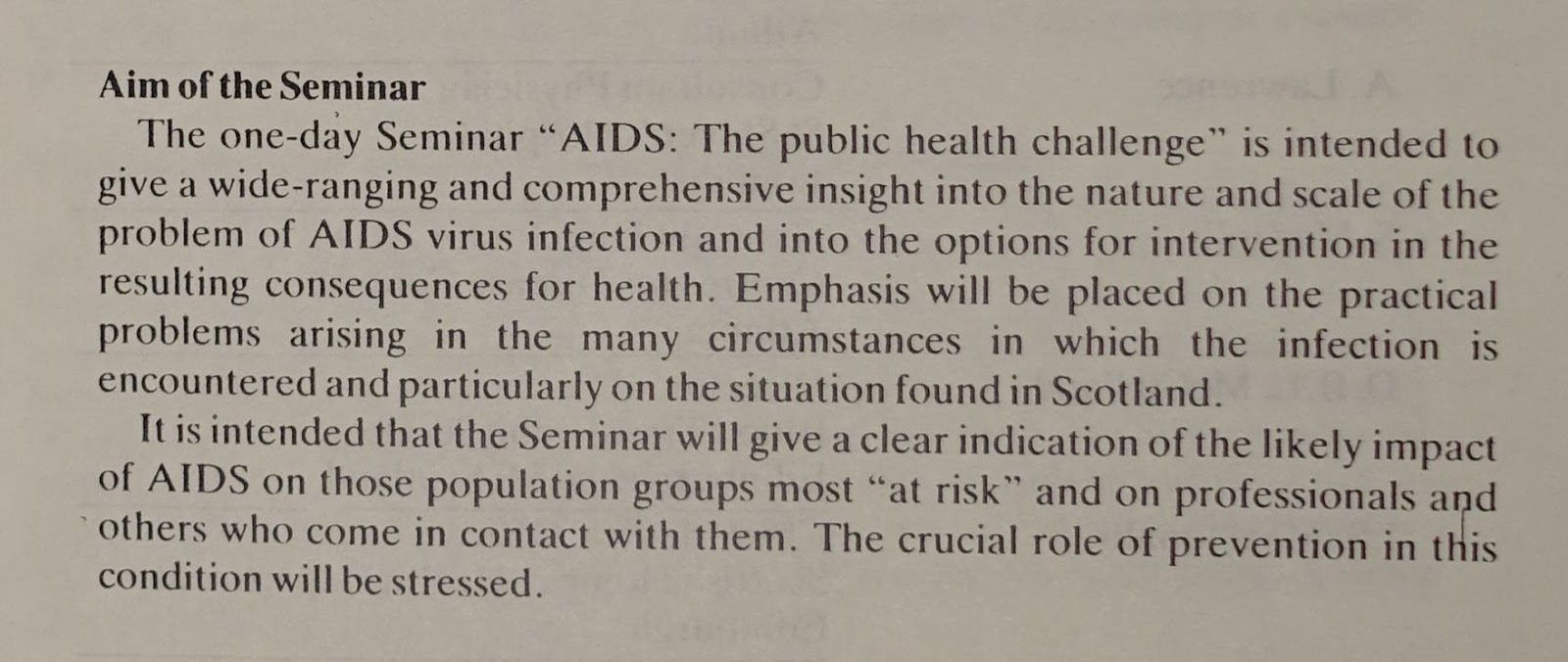
The Public Health Challenge, Outline Programme (GD25/1/2/2/2)
Excerpt from The Public Health Challenge, Outline Programme (GD25/1/2/2/2)
In the early days of the European Collaborative Study, she
was always having to justify herself every time she was asked, “You’ve only got
150 children, why are you needing so much time?”. However, each child needed
follow-up at one week, three weeks, six weeks, and then six-weekly until six
months, three monthly until aged 2 years, and then six to twelve monthly. The
reason for this was that they were looking for signs of infection.
They also had to speak to the mothers in the ante-natal
period to seek their consent and explain the purpose of the study, and they all
were very thankful that somebody was interested in them and their
children. Our colleague, Louise Williams, who’s Archivist at LHSA, did an oral
history interview with Jacquie Mok and Helen Zealley in 2018. In the interview,
Dr Mok recalls that when women ‘were recognised to have HIV during labour,
people would come into their rooms dressed in what they call “space-suits”, and
then auxiliaries would open their door, put their meals in and then shut the
door and run off’. Likewise, Dr Zealley confessed that it was ‘understandable
that there was fear and there was a lot of blood and a lot of unknown’.
AIDS Guidelines for Social Work Personnel, December 1985 (GD59/3/2/2)
We often think of the role of medical staff from a clinical
perspective. But, while Dr Mok was facing an unprecedented challenge, other
associated challenges added pressure to her role: the human element. Jacqui ran
community-based sessions. This means she didn’t wait sitting in her clinic for
parents to show up. She proactively visited households to examine her patients
and this involved encountering all sorts of situations. She recalls that
mothers were always grateful for her visits and would comply with anything she
asked from them. Many of these women were on their own, whereas, in other
instances, Dr Mok would see a man in the house and assume he was the father
without asking any questions. Fathers may or may not join their partners for
the visit. It was rather common that they left the room during the
blood-letting as they couldn’t stand seeing how the medical staff inflicted
pain on the baby by putting a needle into their veins. Likewise, there were
cases when they ended up shouting at her after trying to extract their baby’s
blood several times.

The Sunday Times - "Born survivor", 15 February 1998 (GD59/1/2/1/2)
The Sunday Times - "Learning to live with the HIV virus", 15 February 1998. The page displays a photograph of Dr Jacqueline Mok (GD59/1/2/1/2)
Many of the mothers saw the birth of their child as an
opportunity to stop using drugs, although there would still be mums who would
continue to use them. At the time of the visit, Dr Mok wouldn’t know what state
they would be in. They could be awake, or not, and there was no way to tell
whether they would cooperate.
In those cases where women were deemed unfit to be parents
due to their ongoing use of drugs, Dr Mok had to work with social workers and
foster carers. For this purpose, she ran special training sessions to educate
them about the needs of infected children and the risks they presented to their
families. Some of these children ended up going to school and because of
confidentiality, Dr Mok’s team didn’t disclose that a child was HIV-positive
and, by extension, that the mother was positive too. Instead, they implemented
a universal management of children who could be infected approach to every
school and nursery, which was a success.
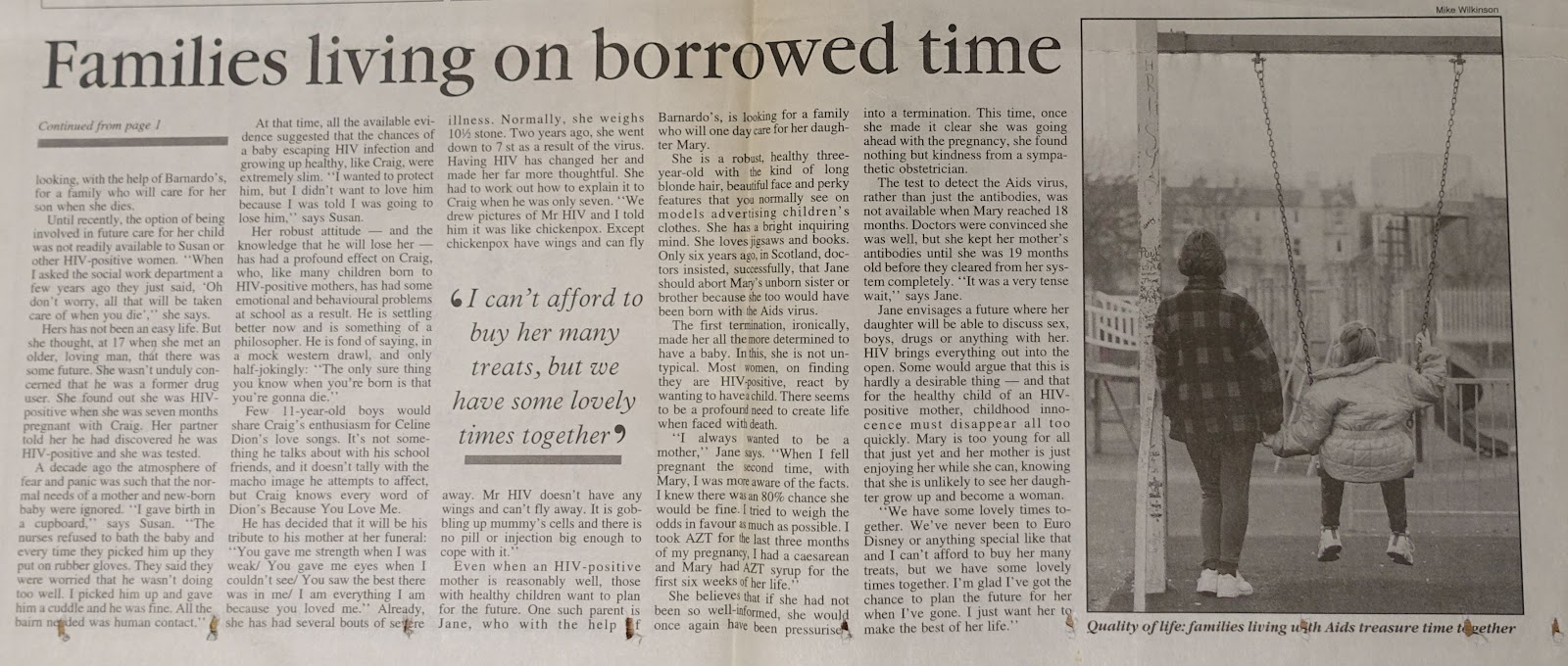
The case of Aileen Ballyntine received plenty of media
attention and made Dr Mok realise that they might have more children affected
by HIV rather than infected by HIV. Ten years down the line HIV-infected
parents were getting ill, before antiretroviral therapy, and they would develop
pneumocystis or suffer from encephalitis. Disclosing their secret to their
children was a very sensitive thing for the mothers to cope with. A lot of
these women, because of their drug use, didn’t have a support network and had
distanced themselves from their families. They lived dysfunctional lives and
were very unsupported. Others would have parents who rejected them. A ‘you
brought it on yourself’ kind of situation. Some grandparents took care of the
children instead of having them become fostered or adopted. In this scenario,
many children born to HIV-positive mothers had behavioural problems, in
particular during their adolescence, as this seemed to be the time when many of
them found out their mum was going to die.

The Sunday Times - "Letting go of mum", 15 February 1998 (GD59/1/2/1/3)
The Sunday Times - "Families living on borrowed time", 15 February 1998 (GD59/1/2/1/3)
In the oral history interview, Dr Mok remembers one
particular case of a child who turned out not to have HIV. The grandfather was
desperately trying to do everything right for his granddaughter, feeling they
had failed their daughter in the past and were trying to make amends. His wife
became very ill and he brought the little girl to Dr Mok since he couldn’t take
care of simple things such as giving her food because he couldn’t cook. He had
relied on his wife all his life to raise their children and now felt powerless.
In other cases, parents could not gather the courage to explain to their
children why they were having their blood taken over the years and asked Dr Mok
to speak to them. There is even a mention of a case when the father wanted to
find and kill the person who gave his wife HIV after she was diagnosed with it.
Dr Mok wore many hats. She was an HIV-specialist doctor, a counsellor, a social
worker…
The mothers’ social spectrum remained a constant during
these years. Unless children were fostered or adopted (this would be by more
structured families), children would grow up within a disadvantaged and
dysfunctional family system. It was in areas like Craigmillar, Niddrie,
Muirhouse, Pilton, and Leith where HIV hit hard. We may think of Leith, for
instance, as this trendy part of Edinburgh nowadays. A place with a lively
cultural scene and full of nice cafes, bars, and restaurants. However, the
reality was way different during the mid-1980s and early 1990s. Think of Trainspotting.
Some of the children from Dr Mok’s cohort became mothers
themselves and coped with varying levels of success. Many mothers continued to
lead an equally dysfunctional life and parenthood didn’t change that. Many of
them are part of a cycle, or a loop, that goes round and round as that’s how
their children are raised. They know no different and follow what their mothers
say and do. Just like any other kid. But, to conclude on a positive note, Dr
Mok stated that those cases who managed to break the cycle of deprivation
managed to do well for themselves.







.TIF)
.TIF)