In this week’s blog, Archivist Louise goes back to class….
Archivists come in all shapes and sizes (literally and metaphorically!)
and from a variety of different backgrounds, but those working in professional
posts during the last few years have one thing in common: a vocational
qualification in record-keeping from one of seven recognised institutions in the
UK and Ireland. One of these qualifications is based at the Humanities Advanced
Technologies and Information Institute (HATII) at the University of Glasgow,
and it’s where three of the four archivists in LHSA trained.
Therefore, when tutor Victoria Stobo asked Project
Cataloguing Archivist Becky and I to speak to her students about the way in
which we deal with confidential data in our everyday work, we were delighted,
although we knew that (as ex-students) it would feel a little strange to be
speaking from the other side of the classroom! Our role as archivists is all
about access, but we need to give that access whilst protecting those people
around whom the archive is built, and both our talks reflected how we do that
in our different fields of work.
As archivist, most of my work with confidential data is
around user services – helping our enquirers with questions about records
closed to general public access. By ‘confidential data’, I mean material that
is covered by either legislation that covers information about living
individuals (i.e. the Data Protection Act) or NHS guidance that protects the patient
and staff records of those now deceased. Since we are one of the largest
medical archives in the UK, holding over one million patient case notes, I deal
with questions about closed archives regularly.
 |
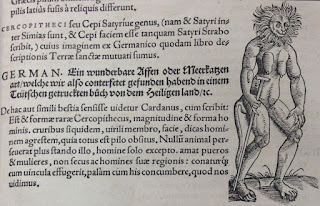
| One of my slides from the talk |
Many people assume that records marked as ‘closed’ are
beyond all access, but that is not necessarily the case. You are entitled to
access any health information that LHSA may hold about you under the Data
Protection Act (1998), for example, as long as you can prove your identity. We can
also apply to the owners of our records, NHS Lothian, for enquirers to see closed
records about other people if they can prove that they have a legitimate reason
for wanting to see them, along with proof that the record subject has given
consent if s/he is living, or that the enquirer can prove the record subject is
deceased.
In our experience, people want to look at confidential
material for two main reasons – either as researchers going through a large
number of records, for whom the identity of individuals is not their main interest,
and genealogists or other interested family members for whom identity of a
person is central. We treat access to otherwise closed records very seriously,
and I explained to the students that applying to see a closed record is far
from a ‘rubber stamp’, but a considered process. I also went through the measures
that we take to keep confidential information secure if an enquirer (such as an
academic researcher in the reading room) is allowed to see a closed record.
When I first started my role as archivist, dealing with
access to closed records was intimidating to say the least, but (as I explained
to the students) working with legislation about access to records is an
essential part of my role and soon became a lot less terrifying and a lot more intriguing!
One of my favourite things about my research with closed records is that I work
with people much closer to the record subject (even the record subject
themselves) – this compression of time is a sharp reminder of the fact that
names recorded in our archive are not just entries in registers but individuals
with their own histories that led them here.
Becky’s role at LHSA is also about access to closed records,
but in terms of the description of those records. As you know from last week’s blog,
Becky is cataloguing tuberculosis case notes in order to give researchers an
intellectual way in to these mostly-closed records. Becky catalogues using
eXtensible Mark-up Language (XML) in order that she can both highlight key
elements of cases for search and hide parts of the description in a public,
online catalogue so that the identities of patients stay private. As Becky
explained, her project (in common with Aline’s work on Norman Dott’s neurosurgical case notes) is designed to give researchers a guide to what these under-used records convey
in order to realise their potential as academic (and genealogical and clinical)
resources.
Becky explained to the students how she thinks of
confidentiality in terms of a jigsaw. There are certain pieces of the puzzle
that she must keep hidden inside a public catalogue in order to protect the anonymity
of patients (such as a name, for example), but there are others (such as the
fact that a person has tuberculosis) that do not in themselves reveal who
somebody is. Even some identifying details (such as a home address) can be
described in more generalised terms (since geography is fairly crucial to infectious
diseases, Becky describes a patient’s origin in terms of electoral districts,
for example). However, Becky has to be on her guard, since sometimes an
apparently innocuous bit of information (like a precise occupation) can slide
the pieces of the jigsaw into place, as neatly demonstrated with these slides:
We got more than a few questions from the aspiring archivists and records managers following our talk – and it
was interesting to see what aspects of our work were of most interest to the
students. All-in-all, an extremely successful morning – and nice to revisit our
former course (although without the assignment deadlines, obviously!).